A multi-institutional team of researchers, including two Northwestern University engineers, has received up to $34 million from the Advanced Research Projects Agency for Health (ARPA-H) to fast-track the development of a low-cost bioelectronic implant to treat patients with obesity and Type 2 diabetes, the agency announced today.
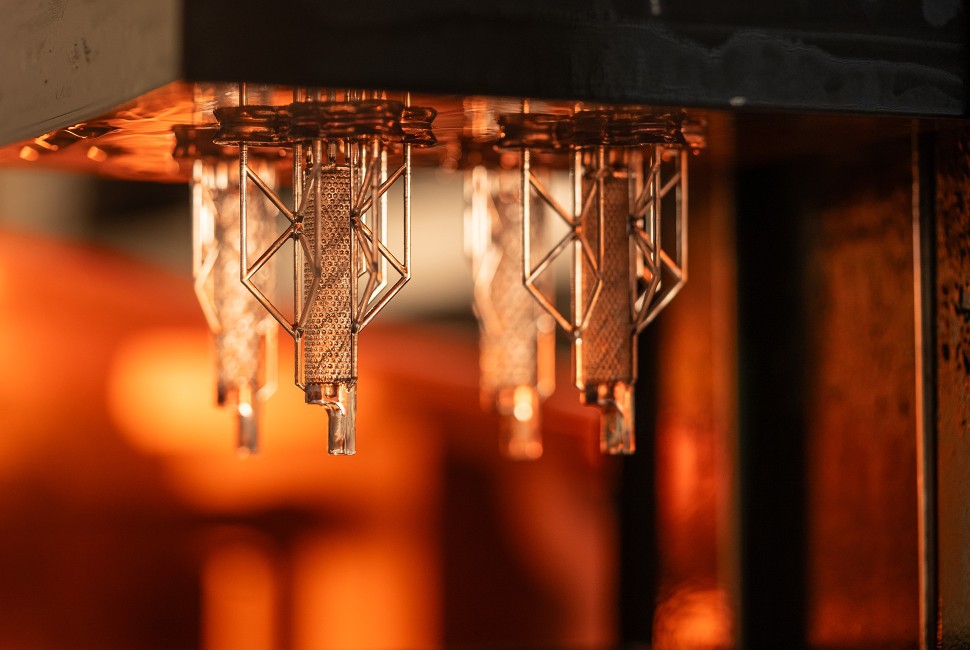
The funding will support a six-year effort to develop and test “Rx On-site Generation Using Electronics” (ROGUE), an implantable device that will deliver a biological therapy on demand to treat obesity and Type 2 diabetes. Measuring just a few millimeters in diameter, the implant will house living engineered cells that synthesize and deliver the therapy when needed — eliminating the need for daily or weekly injections, trips to the pharmacy and careful storage of expensive medications.
“This work builds on the biohybrid work seeded at Northwestern, where we are making regulated therapies based on engineered cell factories that can be controlled and maintained by a bioelectronic device,” said Northwestern’s Jonathan Rivnay, a co-principal investigator of the project who leads device development. “In this work, we aim to develop a minimally invasive living device that can be implanted under the skin and can deliver personalized and regulated therapies.”
Rivnay is a professor of biomedical engineering and materials science and engineering at Northwestern’s McCormick School of Engineering. Josh Leonard, a professor of chemical and biological engineering at McCormick, will lead the development of genetic circuits that make the engineered cells controllable and productive. Rivnay and Leonard are members of the Center for Synthetic Biology and the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
ROGUE builds on two projects that Rivnay co-leads to develop implantable “living pharmacies.” In March 2021, Rivnay received $33 million from the Defense Advanced Research Projects Agency (DARPA) to fund the development of a fully implantable device to control the body’s sleep-wake cycles. Then, in September 2023, Rivnay and collaborators received up to $45 million from ARPA-H to develop a first-of-its-kind implant to sense and autonomously treat cancer.
“Bioelectronic devices offer a myriad of benefits, including adjustable therapy delivery, dynamic monitoring, and reduced biologics healthcare costs,” said Tzahi Cohen-Karni, a professor of biomedical engineering and materials science at Carnegie Mellon University, who is primary investigator of the ROGUE project. “We are leveraging our collective strengths to develop an effective and sustainable solution to reduce the burden of chronic care for two global epidemics — obesity and Type 2 diabetes.”
Rivnay and Leonard are two of ROGUE’s 19 co-principal investigators in the collaborative team, which includes engineers, physicians and multidisciplinary specialists in synthetic biology, materials science, electrical engineering and other fields. The other principal investigators represent the Georgia Institute of Technology; Rice University; University of California, Berkeley; Mayo Clinic and Bruder Consulting and Venture Group.
Established in 2022, ARPA-H is a new federal funding agency that supports research with “the potential to transform entire areas of medicine and health.” ROGUE is funded under ARPA-H’s REACT program and includes funding for a first-in-human clinical trial for patients with obesity and Type 2 diabetes. Trial preparation is slated to begin in the project’s fifth year.