Certain racial and ethnic minorities develop type 2 diabetes at a younger age than white Americans, meaning current diabetes screening and prevention practices for them may be inadequate and inequitable, reports a new Northwestern Medicine study.
American adults are diagnosed with type 2 diabetes at an average age of 50 years old, but the 3,022-participant study found the average age at diagnosis was four to seven years earlier in non-Hispanic Black and Mexican American adults compared with non-Hispanic white adults. More than 25% of non-Hispanic Black and Mexican American adults with diabetes reported a diagnosis before turning 40.
The study was published today, Sept. 7, in the journal JAMA Internal Medicine.
Knowing when certain populations typically get diagnosed with a disease can help inform when doctors start screening to implement treatments that can slow or stop progression of the disease. Those screenings are covered under insurance plans when they are recommended by the U.S. Preventive Services Task Force (USPSTF), the national independent panel of experts that systematically reviews evidence to develop recommendations for clinical preventive services.
“The earlier you can screen, the better, but the biggest barrier to screening is the tradeoff for cost and benefit. Screening too early when a disease is not prevalent is not cost effective,” said corresponding author Dr. Sadiya Khan, assistant professor of medicine and of preventive medicine at Northwestern University Feinberg School of Medicine. “The earlier you identify disease can make screening have the most impact when intervention may have greater benefit. Not doing so may contribute to substantial disparities in diabetes outcomes.”
Burden of diabetes has shifted earlier in the lifespan
Preventive measures such as nutrition counseling, weight-loss and physical-activity programs and the Centers for Disease Control and Prevention’s National Diabetes Prevention Program can prevent or delay the onset of diabetes. The study findings suggest that greater prevention efforts are needed at younger ages in underserved communities to help narrow the gap in age at diabetes diagnosis, said first study author Michael Wang.
“Sixteen percent of non-Hispanic Black and 21% of Mexican American adults with diabetes reported a diagnosis before 35 years old in our study, which suggests that reaching young adults in these groups for preventive care is needed to address a critical period when diabetes is developing,” said Wang, a fourth-year medical student at Feinberg.
The findings also highlight the need to recognize and address how social determinants of health – the economic and social conditions that influence individual and group differences in health status – lead to increased risk among minority populations and reflect an underlying health inequity, the study authors said.
20% people with diabetes don’t know they have it
The study was a cross-sectional analysis of data from the National Health and Nutrition Examination Survey from 2011 to 2018. This survey provides population-level data on age at the time of diagnosis in those who are aware of their diagnosis, but about 20% of people with diabetes do not know they have the disease, Wang said, which is why it is important to implement broader screening at younger ages.
The USPSTF recently announced new guidelines that lowered the recommended age from 40 to 35 to start screening adults with overweight or obesity for type 2 diabetes. Future research should consider whether even earlier screening is indicated among individuals with exposure to social risks, the study authors said.
“Unless your blood sugar climbs to an alarming level where you’re experiencing fatigue, frequent urination and symptoms of hyperglycemia, your diabetes may remain undetected for quite a while,” Khan said.
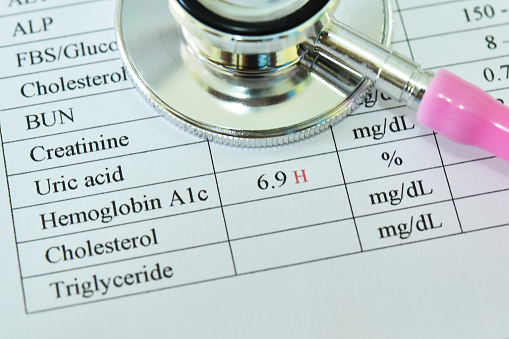
To screen for diabetes, doctors most commonly administer a blood test known as a hemoglobin A1C (HbA1c) test, which measures a person’s average blood sugar levels over the prior three months. Less than 5.7% HbA1c is normal; 5.7-6.4% is prediabetic and 6.5% is diabetic.
“We, as physicians, are always telling people to ‘know your numbers,’ which has historically been about blood pressure and cholesterol, but it should be expanded to include HbA1C,” Khan said.
Other Northwestern co-authors include Dr. Nilay Shah, Professor Mercedes Carnethon and Dr. Matthew O’Brien.