Researchers at Northwestern Medicine have taken the first step in bioengineering the human uterus to treat endometriosis, uterine-factor infertility and endometrial cancer.
The study is the first to demonstrate that induced human pluripotent stem (iPS) cells can be reprogrammed to become healthy uterine cells for potential placement in the uterus. Made from a person’s own readily available cells, iPS cells can potentially be manipulated to fix defects within other, disease-causing cells. The healthy cells are then optimal for an auto-transplant that won't be rejected by the person’s immune system.
The study was published Nov. 1 in the journal Stem Cell Reports.
This is huge. We’ve opened the door to treating endometriosis.”
Senior study author, Northwestern Medicine
Women with abnormal endometrial cells may experience infertility because these defective endometrial cells are not receptive to an implanting embryo. This study opened the avenue for replacing these defective endometrial cells with normal ones derived from a woman’s own skin or blood.
“This is huge. We’ve opened the door to treating endometriosis,” said senior author Dr. Serdar Bulun, who has been researching treatments for endometriosis for the past 25 years. “These women with endometriosis start suffering from the disease at a very early age, so we end up seeing young high school girls getting addicted to opioids, which totally destroys their academic potential and social lives.”
Bulun is the chair of the department of obstetrics and gynecology at Northwestern University Feinberg School of Medicine and a Northwestern Medicine physician.
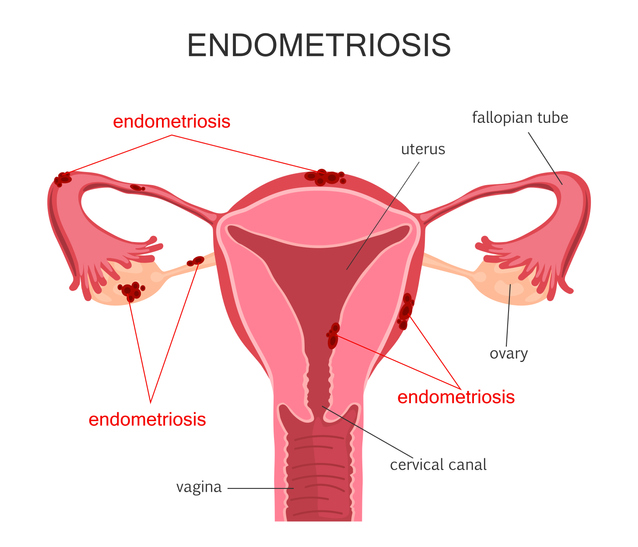
Endometriosis occurs when the endometrial cells in a woman’s uterus do not respond to an adequate amount of an implantation hormone called progesterone.The abnormal cells, called defective endometrial stromal fibroblasts, travel through the fallopian tubes, then onto the lower abdominal tissues and the ovaries. Extra-uterine growth of endometrium-like tissue results in severe pelvic pain, infertility and development of adhesions and increases the risk for ovarian cancer.
Now that this study has demonstrated that these cells can be reproduced and respond properly to progesterone, the next step would be to replace the diseased cells in the uterus with these newly programmed, healthy uterine cells, Bulun said.
As cell-based therapy methods continue to improve, the defective cells that cause inflammation and pain in the uterine cavity of endometriosis patients would be replaced with the normally programmed cells in the future. This way, pain would be eliminated long-term. Moreover, the newly formed normal endometrium would be more receptive to an implanting embryo.
“One day we hope to make a whole uterus using this cell-based treatment employing the patient’s own iPS cells,” Bulun said.
Uterine transplantation has been tried, but the biggest obstacle to success has been the rejection of someone else’s uterus with the patient’s immune response. This problem could be solved if a whole uterus can be bioengineered by populating a scaffold with the patient’s own iPS cells reprogrammed to form a uterus. However, this is a long shot, Bulun warns.
Dr. Kaoru Miyazaki at Northwestern conducted the key experiments for this study. Both Bulun and Miyazaki consulted closely with their co-author, Dr. Tetsuo Maruyama from Keio University in Tokyo, Japan.
Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health funded this study by extending grant HD38691 to Bulun.