
Jonathan Rivnay
Co-principal investigator
Professor of biomedical engineering and materials science and engineering
Project receives ARPA-H contract worth $45 million over five-and-a-half years
EVANSTON, Ill. — A multi-institutional team of researchers, including Northwestern University scientists, has received $45 million from the Advanced Research Projects Agency for Health (ARPA-H) to fast-track the development of a first-of-its-kind implant to sense and treat cancer, the agency announced today.
Established in 2022, ARPA-H is a new federal funding agency that supports research with “the potential to transform entire areas of medicine and health.” Northwestern’s project is the second program funded under ARPA-H’s inaugural Open Broad Agency Announcement solicitation for research proposals.
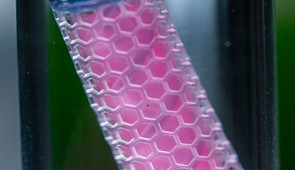
The funding will support a five-and-a-half-year effort to develop and test a device that can sense inflammatory markers associated with cancer and then autonomously deliver immunotherapy. Measuring just 1 centimeter in diameter, the small implant will house living engineered cells that both synthesize and deliver therapies when needed.
During the first four years, the researchers will develop the technology and test it on small and large animal models. In the fourth year, the researchers will begin human clinical trials, starting with patients who have recurring ovarian cancer.
The end goal is to develop a device to provide personalized therapy, tailored to individual cancer patients.
“From a clinical perspective, this could be a game-changing approach to cancer therapy,” said Northwestern’s Jonathan Rivnay, a co-principal investigator on the project who leads device development. “It’s personalized, multi-modal and could improve access to care. This concept of a regulated cell-based therapy also is exciting for other areas of medicine, and this project allows us to develop the toolbox of components needed to make it a reality.”
Rivnay is a professor of biomedical engineering and materials science and engineering at Northwestern’s McCormick School of Engineering. Shana Kelley, the Neena B. Schwartz Professor of Chemistry and Biomedical Engineering at Northwestern, will develop new sensor chemistries and evaluate sensor performance. Kelley has appointments in McCormick, the Weinberg College of Arts and Sciences and Northwestern University Feinberg School of Medicine and is co-leader of the Cancer & Physical Sciences Program of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
Working at the leading edge of bioelectronics and synthetic biology, Rivnay’s lab develops soft, biocompatible electronics equipped with living engineered cells that can synthesize and deliver therapeutic biomolecules. As a part of this work, Rivnay also leads a Defense Advanced Research Projects Agency (DARPA) funded project to develop a fully implantable device to control the body’s sleep-wake cycles. Now, he joins a team — comprising engineers, physicians and multidisciplinary specialists in synthetic biology, materials science, immunology, oncology, electrical engineering and artificial intelligence — to develop a similar approach for treating cancer.
According to the researchers, the implant could dramatically improve immunotherapy outcomes for patients with ovarian, pancreatic and other difficult-to-treat cancers — potentially slashing U.S. cancer-related deaths by 50%.
“Instead of tethering patients to hospital beds, IV bags and external monitors, we’ll use a minimally invasive procedure to implant a small device that continuously monitors their cancer and adjusts their immunotherapy dose in real time,” said Rice University bioengineer Omid Veiseh, principal investigator on the ARPA-H cooperative agreement. “This kind of ‘closed-loop therapy’ has been used for managing diabetes, where you have a glucose monitor that continuously talks to an insulin pump. But for cancer immunotherapy, it’s revolutionary.”
One of the project’s biggest challenges is to overcome the harsh environment inside the human body, which is inhospitable to electronics. Not only is the body constantly moving, it also is filled with fluids that could corrode the implant. Working with Kelley, Rivnay will explore methods to leap this hurdle.
“Sensing in the complex environments in the body is a well-known, challenging task,” Rivnay said. “The Northwestern-led effort will tackle these challenges with the goal of stable and continuous monitoring of biochemical signals that will provide real-time readouts of cancer progression and therapy — rather than sparse snapshots that are more typical in current practice.”
In addition to Northwestern and Rice, the team includes members from Carnegie Mellon University; Georgia Institute of Technology; the University of Texas MD Anderson Cancer Center; Stanford University; the University of Houston; Johns Hopkins University; Chicago-based startup CellTrans; and New York City-based Bruder Consulting and Venture Group.

Co-principal investigator
Professor of biomedical engineering and materials science and engineering