Embed Video:
<iframe width="560" height="315" src="https://www.youtube.com/embed/8qzuE1t_zHU" frameborder="0" allow="accelerometer; autoplay; encrypted-media; gyroscope; picture-in-picture" allowfullscreen></iframe>
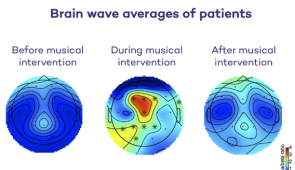
Brain waves of distressed, anxious patients slow to meditative state as violist plays
CHICAGO --- Improvisatory clinical viola music calms agitated epilepsy patients — as seen in their brain waves — when they are hospitalized in the epilepsy-monitoring unit, reports a new Northwestern Medicine pilot study.
Patients with epilepsy endure difficult conditions in the hospital to undergo testing. They must temporarily stop or decrease their medications during their hospitalization to provoke seizures. Many feel distressed and anxious. Some are so uncomfortable, they cannot complete their testing.
But when these patients listened to improvisatory music — a violist playing live music who responded to their state of agitation in real time — the patients’ brain waves (as monitored on an EEG) slowed to a calmer state, allowing the testing to continue. Patients also reported decreased feelings of stress and anxiety after their clinical music experience.
“Their brains went into a meditative state,” said lead investigator Dr. Borna Bonakdarpour, associate professor of neurology at Northwestern University Feinberg School of Medicine and a Northwestern Medicine neurologist. “When they engaged with the real world, such as watching a TV show or browsing social media on their phone, their brain frequency was an average of 12 or 13 (beta waves) Hertz, but after the music it dropped to an 8 or 9, which is the alpha state.”
The study was published Sept. 1 in Frontiers of Neurology.
The viola was chosen for this research due to its pitch range reflecting the human “safe” vocal range, which is the two middle octaves. Research shows this range, used for lullabies, activates the calming systems of the brain.
“There has been a scarcity of non-pharmacological interventions for epilepsy patients in the hospital, and we show that the patients benefited significantly from music intervention,” Bonakdarpour said. “Importantly, the patients’ self-reports correlated with objective EEG changes, which is something that had not been previously done in an epilepsy-monitoring unit.”
The study with five patients was small, but Bonakdarpour is planning a larger clinical trial with 30 to 50 patients.
The impact of the findings may apply to patients in the hospital for other reasons, Bonakdarpour said.
“Music as a clinical tool is underutilized in outpatient settings and in hospitals,” he said.
During the pilot study, 21 patients with epilepsy were identified as suitable for the trial. Five of these individuals were reported by the nursing and social work staff to have significant distress and were included in this study to receive the intervention. Listening to recordings of their favorite songs alone did not seem to be effective for these patients.
Participants in the study received a personalized 40-minute live music session over FaceTime by a clinically trained violist in consultation with a music therapist.
Clinically designed improvisatory music has simple meandering melodies played at a slow tempo. The improvisation is slow and meterless, played in the form of two-minute-long statements with an ending that tapers to silence.
The music was offered as part of the Northwestern Medicine Telemusic Intervention program during COVID-19 lockdown to relieve patients’ distress in the Northwestern Memorial Hospital neurosciences unit. The results of the broader study included 87 sessions during a three-month period.
Northwestern co-authors include: Guangyu Zhou, Daniel Huang, Catherine Vidano, Stephan Schuele, Christina Zelano and Clara Takarabe.
The title of the article is "Calming Effect of Clinically Designed Improvisatory Music for Patients Admitted to the Epilepsy Monitoring Unit during the COVID-19 Pandemic: A Pilot Study."
The research is funded by National Institutes of Deafness and other Communication Disorders (NIDCD) grant R01-DC-018539 of the National Institutes of Health and Northwestern’s department of neurology philanthropy.
<iframe width="560" height="315" src="https://www.youtube.com/embed/8qzuE1t_zHU" frameborder="0" allow="accelerometer; autoplay; encrypted-media; gyroscope; picture-in-picture" allowfullscreen></iframe>