The viral ALS Ice Bucket Challenge a few years ago raised major funding that resulted in the discovery of new genes connected to the disease. One of those genes is NEK1, in which mutations have been linked to as much as 2% of all ALS cases, making it one of the top-known causes of the disease.
But it wasn’t known how the mutated gene disrupts the function of the motor neuron and causes it to degenerate and die.
Northwestern Medicine scientists have discovered for the first time how this mutated gene leads to ALS (amyotrophic lateral sclerosis).
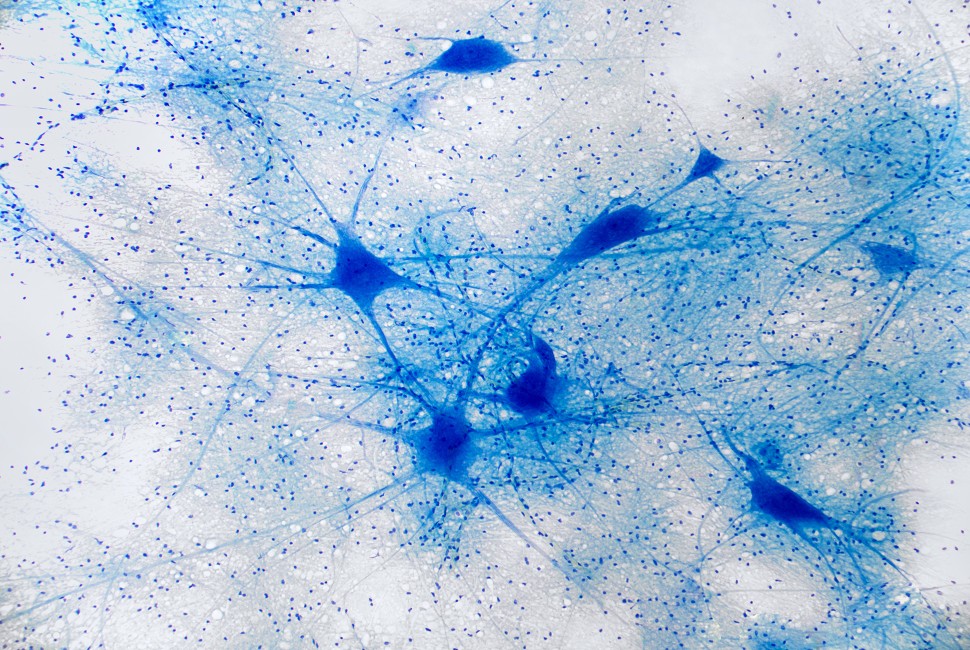
The investigators found the mutation causes two problems in the neuron. The first is that it causes the structures supporting the axon in the neuron to become less stable and susceptible to collapsing. (The axon is the thinner-than-a-human-hair cable leading from the cell that sends electrical messages to other neurons.)
The second problem the scientists discovered is that the mutation disrupts the ability of the neuron to import cargo in the form of RNA or proteins into its nucleus, a process called nuclear import. Without the import of RNA – which carries instructions from the DNA – and critical proteins, the operational role of nucleus for the cell’s function is disrupted.
The paper was published August 16 in Science Advances.
“By illuminating these two pathways, we’re suggesting these are great therapeutic targets for the disease,” said study lead author Evangelos Kiskinis, assistant professor of neurology and neuroscience at Northwestern University Feinberg School of Medicine.
“This discovery is important because a major breakthrough in ALS research in the last few years was discovering that nuclear import is disrupted in other forms of genetic ALS,” Kiskinis said. “We are linking this new cause of ALS to other genetic causes in which the same process is disrupted.”
A major unaddressed question in the field is whether ALS is one disease or a collection of genetically distinct smaller versions under the “umbrella” of the same clinical problems, Kiskinis said.
“Our discovery — of the same destructive mechanisms in other genetic forms of ALS — leads us to believe this is the same disease,” Kiskinis said. “This new awareness is critical to developing treatments and for designing optimal clinical trials targeting specific ALS patient populations.
ALS is a devastating neurodegenerative disease in which the upper and lower motor neurons in the brain and spinal cord dysfunction and die. It results in the loss of voluntary muscle movement, which leads to paralysis and eventual death.
The structural components of the nerve’s axon, which are destabilized in ALS, are microtubules. Kiskinis knew anti-cancer drugs such as paclitaxel, which target and stop the dividing of cancer cells, help stabilize the microtubules. So, the Northwestern team tested these anti-cancer drugs in ALS models of human neurons (made from ALS patients’ stem cells). The drugs stabilized the microtubules in vitro and restored the ability of nerve cells with the ALS mutation to function.
Kiskinis says it would be exceptionally challenging to use such anti-cancer drugs to treat ALS patients as they would likely have severe side effects, and a very narrow dose range as over-stabilizing microtubules can be toxic to neurons. However, the findings serve as proof of principle.
“This suggests that stabilizing microtubules is a rational therapeutic approach in ALS,” Kiskinis said.
Kiskinis and his team are currently working on understanding more precisely how NEK1 regulates microtubules and nuclear import in human neurons. They also are developing approaches to increase the function of NEK1 to prevent the degeneration of the neurons in ALS.
Other Northwestern authors include Elizabeth McKenna, Jacob Mann, Vasileios Papakis, Francesco Alessandrini, Ryan Mayers, Hannah Ball, Evan Kaspi, Katherine Lubinski and Liana Tellez.