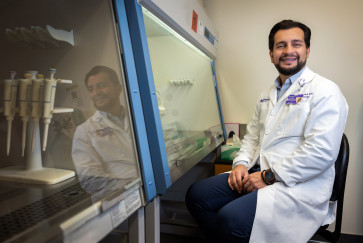
Sterling Elliott is an assistant professor of orthopaedic surgery at Northwestern University Feinberg School of Medicine in Chicago and a Northwestern Medicine pharmacist.
I was sitting in a suburban Chicago middle school a few years ago, talking to the mom of one of my son’s friends, when she told us she had been in a car accident that badly injured her shoulder. She’d recently had a successful surgery on it and was prescribed opioids.
Very nervous, she looked at me, a pharmacist, and I could tell something was weighing on her. “Am I going to get addicted to the pain meds?” she asked.
That’s when it hit me: People don’t get how to think about opioids.
There’s so much fear surrounding opioids, and rightly so. The U.S. is mired in a public health catastrophe that’s killing way too many of us, especially our teens. In 2021, more than 107,000 Americans died of a drug overdose, with roughly 75% of those coming at the hands of opioids.
Nancy Reagan first championed the “Just say no” slogan 40 years ago, and we’ve been following the “drugs-are-bad” philosophy in this country ever since. But it’s gotten us nowhere in this public health crisis. We need to flip the script.
The fact is we need opioids — let’s face it, they’re the best pain-management tool we currently have at our disposal. But the even bigger problem is we as patients don’t know how to responsibly take them. And even more problematic, we as health care providers are still struggling to help patients navigate when they’re needed and when it’s time to get rid of them.
The reason is because opioids are almost too good at what they do. Their main purpose is to block a target in your brain, which masks the intensity of your pain. If we double the dose of your opioid, you should get about twice the pain relief. But at the same time, the opioids cause dopamine to be released in the brain, which is what feeds the brain’s reward center and causes you to crave more of the drug.

And therein lies the problem: Dopamine’s effects differ from person to person. In some people, just a little more opioid may cause a massive surge of dopamine, even larger than the dose increase. While in others, the surge in dopamine happens slowly over time, and the patient doesn’t even realize it. There’s no rhyme or reason, and it’s often hard for health care providers to tell who’s at greater risk.
Many people who find themselves in the throes of addiction never intended to get there. The reward-seeking drive keeps pushing them toward more and more. They make bad decisions, and for an alarming number of people, it leads to a deadly dose of unknown fentanyl, a synthetic opioid that is pervading the illegitimate drug supply. Far too many people are dying from it without ever intending to use it.
So what can we do?
A little over two years ago, I launched a program at Northwestern that put some of the things I’ve written about as an academic into action. In partnership with my friends and colleagues in orthopaedics, we’ve started going from room to room before patients even have surgery to teach them how to think differently and practically about managing their pain after surgery.
We’ll say, “You’re going to have some surgery. There will be pain, but I don’t want you to think about how bad it feels (0-10). Instead, let your functional abilities (or lack thereof) drive the need for your opioid pain medications.”
We ask them to consider these critical questions throughout their recovery: Can they get out of bed in the morning, move around with limitations, go to the bathroom, eat something, move throughout their day, sleep at night. Finally, are they a reasonable person to be around when they’re awake and recovering? If they can answer yes to all seven questions, they’re functioning with pain after surgery, even though the pain may be difficult.
We also teach patients how to choose between medications that aren’t opioids —ibuprofen, acetaminophen, etc. — when the pain is NOT hampering their function. What does the pain feel like? If it’s pressure and stiffness, swelling or inflammation, we steer them toward ibuprofen. If the pain is just there and they need it to be less aggravating, we steer them toward acetaminophen. Every time you know the pain is there, and if you’re answering yes to those seven questions, you know it’s not affecting your ability to function, and, therefore, the opioid is not the tool in your toolbox you should be using.
Most importantly, we teach them when to know they don’t need opioids and how to get them out of the house. If they’re to the point where the pain doesn’t merit asking those seven questions, it’s time to get rid of your opioid. There are kiosks and take-back days (I lead the semi-annual effort for Northwestern Memorial Hospital) where patients can drop them off and they can be disposed of safely.
It’s an innovative movement we’ve created, and I’m convinced it’s the missing link to help stem the tide of opioid overdose deaths. We looked at our success when we launched this program and found patients who received our teaching asked for fewer refills at a rate of 3.5%. The latest estimates show Americans receive 250 million opioid prescriptions every year. At this rate, that means the total would drop by roughly 8.75 million prescriptions every year. If we want to make a difference, this movement needs to infiltrate every health care center across the country.
We’re learning more about these drugs and how to responsibly use them. We’ve learned the key is to help patients swallow fewer pills.