Dr. Prakash Jayabalan has long pondered why more non-operative treatment options aren’t available to patients with knee osteoarthritis (OA), particularly because it is the most common cause of disability in the U.S.
“Doctors perform approximately 1 million surgical knee replacements each year,” he said. “Of course, a proportion of these people need surgery. However, I’ve always felt that a lot of patients with OA are getting knee replacements much sooner in life than needed.”
Dr. Jayabalan is the physician-scientist director of the Nancy W. Knowles Strength + Endurance Lab at Shirley Ryan AbilityLab and assistant professor of physical medicine and rehabilitation at Northwestern University Feinberg School of Medicine.
The question — how to help patients with knee OA feel better without surgery — has prompted two research studies he leads at Shirley Ryan AbilityLab. One is a new test to identify OA earlier. And the other is the novel use of equipment to help patients with OA get the full benefits of exercise without pain.
Identifying knee OA earlier
Staying active is the best way for a patient to keep OA from getting worse. Yet, one of the biggest challenges of current knee OA treatment practices is that diagnosis typically happens only after a patient is in such severe pain that activity is difficult.
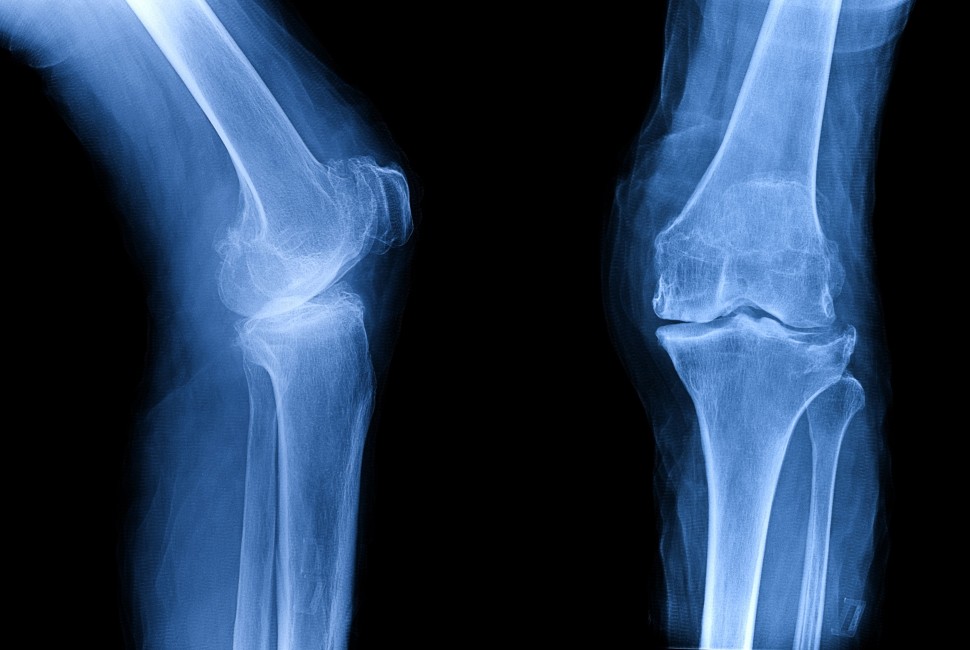
“Right now, I can diagnose patients with knee OA using an X-ray and send them for physical therapy, pain management and maybe injections,” Dr. Jayabalan said. “However, by that point, the OA is already far down the line. I don’t have anything to prescribe that will prevent its progression.”
To help doctors diagnose knee OA much earlier, Dr. Jayabalan and his lab team are developing a new protocol that he describes as a “cartilage stress test.”
“We have the patient exercise to put stress on the joints, and then we measure the body’s responses to that stress by looking at blood- or synovial-based biomarkers,” he said.
With early diagnosis, we could prescribe an individualized, preventive exercise program.”
Shirley Ryan AbilityLab
The design of the cartilage stress test relies on two novel aspects to measure the metabolic state of joints. First, it uses a real-time approach. Dr. Jayabalan’s team takes blood during periodic intervals using an IV line while the patient is walking on the treadmill, instead of relying on blood taken pre- and post-evaluation.
Second, the test uses a special treadmill that provides a mediolateral tilt of up to 10 degrees. This angle creates individualized stress loads on each joint.
This new protocol could lead to individualized treatment plans for patients at risk of early OA — for example after anterior cruciate ligament (ACL) reconstruction — while they are still relatively healthy, years before their joints start hurting. Ideally, early intervention will delay or even eliminate the need for joint replacements.
“We generally tell patients to walk 30 minutes a day, five times per week,” he said. “My goal is to identify an optimal prescription for each patient that would prevent disease progression. With early diagnosis, we could prescribe an individualized, preventive exercise program.”
Taking the load off
For patients with joint pain caused by advanced knee OA, an exercise prescription consisting of even the simplest tasks, such as walking for 30 minutes, can present an overwhelming challenge. Dr. Jayabalan’s lab is pursuing a hopeful alternative — use of an anti-gravity treadmill that allows knee OA patients to walk longer without increasing joint pain, while still reaping the full cardiac benefits.
Anti-gravity treadmills are increasingly more common in physical therapy regimens for patients recovering from ACL and other knee injuries. These devices enclose the patient’s lower body in a vacuum, and allow the therapist to vary the body-weight load that patients feel as they walk or run on the treadmill.
In a pilot study, Dr. Jayabalan’s team observed 30 patients with knee OA over the course of two 30-minute sessions. In one session, research subjects attempted to walk for 30 minutes on a treadmill at their full body weight. In the second, they attempted the same goal on an anti-gravity treadmill, set to reduce their body weight by 50 percent. Study results were overwhelmingly positive.
“We’ve had subjects who felt they could not walk 15 minutes on a flat surface — but when they were walking on the anti-gravity treadmill, and we reduced their body weight, they were able to walk the full 30 minutes,” he said. “The reduced body weight enabled them to walk longer due to significantly less joint pain, and they got the full cardiovascular benefit of 30-minutes’ exercise. Additionally, their biomarker responses indicated significantly less stress placed on their cartilage and improved gait parameters.”
Clearly, anti-gravity treadmills are showing promise for these patients, but they are expensive. The good news, Dr. Jayabalan said, is that there is a much simpler, more affordable and readily available way to reduce load on arthritic joints — aquatic therapy.
“A pool can un-weight the patient, too,” he said. “Buoyancy affords significant biological and biomechanical benefits that potentially could allow someone with knee OA to walk without joint pain for longer.”
The Shirley Ryan AbilityLab, formerly the Rehabilitation Institute of Chicago (RIC), is the global leader in physical medicine and rehabilitation for adults and children with the most severe, complex conditions — from traumatic brain and spinal cord injury to stroke, amputation and cancer-related impairment. It has been designated the “No. 1 Rehabilitation Hospital in America” by U.S. News & World Report every year since 1991. In 2017, RIC became Shirley Ryan AbilityLab in recognition of a transformative gift from Patrick G. and Shirley W. Ryan.