Post-COVID pain or weakness? MRI can pinpoint nerve damage
Advanced imaging can diagnose nerve/muscle injuries and guide treatment decisions
- Link to: Northwestern Now Story
After recovering from COVID-19, some patients are left with chronic, debilitating pain, numbness or weakness in their hands, feet, arms and legs due to unexplained nerve damage. A new Northwestern Medicine study shows how advanced imaging technology can pinpoint what may have caused patients’ nerve damage and help determine the best course of treatment.
“Let’s say you have numbness in your fingers. That might actually be due to problems in your neck, elbow or wrist, and the best way to figure it out is with an MRI or ultrasound,” said lead author Dr. Swati Deshmukh, assistant professor of radiology at Northwestern University Feinberg School of Medicine and a Northwestern Medicine radiologist. “We offer advanced imaging that shows even really, really small nerves, which helps us localize where the problem is, assess the severity and suggest what might be causing it."
This is the first known publication to summarize how these advanced imaging techniques can help physicians identify and treat nerve damage in COVID-19 patients. The study will be published December 1 in the journal Radiology.
Two new causes of nerve damage
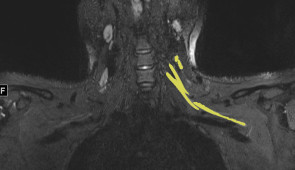
Previous research from Northwestern and Shirley Ryan AbilityLab found COVID-19 patients can experience nerve damage after being flipped onto their stomachs (prone positioning) in the ICU as a life-saving measure to help them breathe. This new paper demonstrates how advanced imaging aids this cohort of patients as well as two additional patient cohorts with COVID-19-related nerve damage:
- Secondary to an inflammatory immune response that attacked the nerves or
- From a hematoma (when blood collects outside of the blood vessels).
“Similar to how the body’s immune response attacks the lungs in severe COVID cases, some patients have an immune response that affects their nerves,” Deshmukh said. “Another group of patients developed hematomas as a complication from the blood thinners they were treated with when they had COVID.
I want physicians and patients to be aware of the diagnostic options available due to recent innovations in technology, and inquire if advanced imaging might be right for them.[/quote]Deshmukh said she hopes the findings will raise awareness of this imaging technology.
“I have to wonder if there are physicians out there who are seeing these otherwise young, healthy patients, and they don’t know exactly what’s wrong and they’re thinking, ‘What am I supposed to do for patients with post-COVID pain and weakness?’” Deshmukh said. “I want physicians and patients to be aware of the diagnostic options available due to recent innovations in technology, and inquire if advanced imaging might be right for them.”
How the technology works
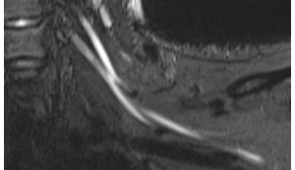
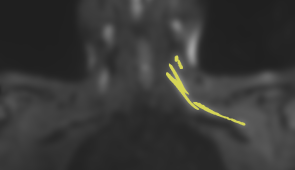
The imaging described in the paper includes ultra-high-resolution ultrasound and MR neurography (MRI of peripheral nerves, which impact the arms and legs). They can help localize where a patient’s problem is, show the severity of nerve damage, how many nerves are affected and if the nerve damage also has impacted the muscles.
The advanced ultrasound technology is new, portable, less expensive and can sometimes be even better at detecting nerve damage than MRI, Deshmukh said. Ultrasound also can be performed on patients who are unable to tolerate MR imaging.
Guiding treatment decisions
If imaging technology discovers nerve damage caused by stretch injury because of prone positioning, Deshmukh said, that patient may be referred to a physician who specializes in rehabilitation or peripheral nerve surgery. If imaging finds nerve damage due to an inflammatory response, the patient may be better served by seeing a neurologist. If imaging reveals nerve damage from a hematoma, blood thinner medications would have to be adjusted immediately and the patient may even have to see a surgeon.
For COVID-19 patients and survivors with neuromuscular complications or “long-hauler” symptoms, imaging can help reveal the problem and guide further treatment.
All patients in the study had tested positive for COVID-19.
Other Northwestern study authors include Dr. Colin K. Franz , Dr. Jason H. Ko, Dr. James M. Walter and Dr. Igor J. Koralnik from the departments of physical medicine and rehabilitation, neurology, plastic and reconstructive surgery, and pulmonary and critical care, respectively.
Multimedia Downloads
MRI shows nerve damage in neck