In recent years, cell and gene therapies have shown significant promise for treating cancer, cystic fibrosis, diabetes, heart disease, HIV/AIDS and other difficult-to-treat diseases. But the lack of effective ways to deliver biological treatments into the body has posed a major barrier for bringing these new therapies to the market — and, ultimately, to the patients who need them most.
Now, Northwestern University synthetic biologists have developed a flexible new platform that solves part of this daunting delivery problem. Mimicking natural processes used by viruses, the delivery system binds to target cells and effectively transfers drugs inside.
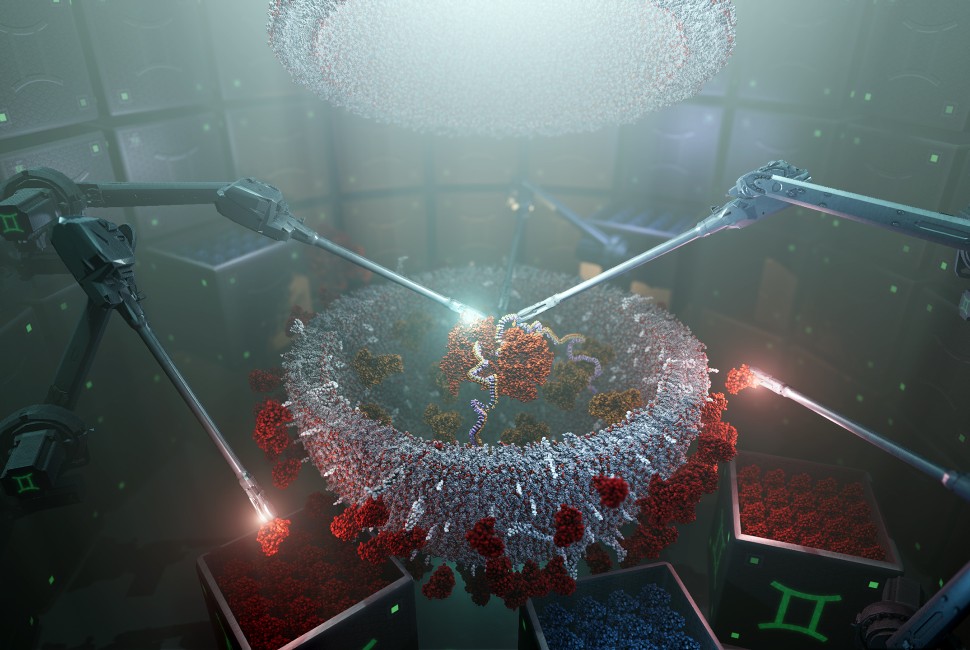
The workhorses behind this new platform are extracellular vesicles (EVs) — tiny, virus-sized nanoparticles that all cells already naturally produce. In the new study, researchers used the powerful approach of synthetic biology to build DNA “programs” that — when inserted into “producer” cells — direct those cells to self-assemble custom EVs with useful surface features. The programs also direct cells to produce and load the EVs with biological drugs.
In proof-of-concept experiments, the particles successfully delivered biological drugs — in this case CRISPR gene-editing agents that knocked out a receptor used by HIV — to T cells, which are notoriously difficult to target. The researchers also hypothesize the system should work for many drugs and many types of cells.
The research was published in the journal Nature Biomedical Engineering. It marks the first study to successfully use EVs to deliver cargo into T cells.
“The genomics revolution has transformed our understanding of the molecular bases of many diseases, but these insights have not resulted in new medicines for one fundamental reason: We lack the technology needed to deliver targeted medicines to specific sites in the body where they are needed,” said Northwestern’s Joshua N. Leonard, who led the study. “These shared delivery challenges are holding us back. By making broadly enabling delivery platforms available, we can remove a huge amount of risk and cost from bringing new drugs to clinical trials or to market. Instead of designing a new delivery system every time a company makes a new drug, we hope that they can instead use modular, reconfigurable platforms like ours, thus accelerating the rate at which gene and cell therapies are developed and evaluated.”
A synthetic biology pioneer, Leonard is a professor of chemical and biological engineering at Northwestern’s McCormick School of Engineering and a key member of the Center for Synthetic Biology (CSB) and of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. Working with Northwestern’s Innovation and New Ventures Office, Leonard launched Syenex in 2022 to help solve drug delivery for cell and gene therapy developers. Syenex is one of 12 startups housed at the Querrey InQbation Lab, Northwestern’s new incubator. The multidisciplinary team includes Julius Lucks, a professor of chemical and biological engineering at McCormick and CSB member, and Judd Hultquist, an assistant professor of medicine (infectious diseases) and microbiology-immunology at Northwestern University Feinberg School of Medicine.
The promises and challenges of targeted drug delivery
By replacing faulty genes or delivering healthy new genes or cells into a patient, gene and cell therapies hold promise for treating a wide range of diseases. Using a delivery vehicle, gene therapies enter the body to transfer genetic material into specific cells to treat or prevent disease. Cell therapies use a similar approach but transfer full cells, which are typically modified outside the body before being administered.
In the most successful cases, viral vectors — which use parts derived from viruses but cannot cause an infection — have served as the delivery mechanism for both cell and gene therapies. But this strategy comes with limitations. The immune system sometimes recognizes virus parts as foreign and blocks such vectors before they deliver their cargo.