First there was COVID-19 lung damage. Then came reports of cardiovascular complications in patients with the virus. Now, the pandemic is highlighting how certain populations, namely African-Americans, in some cities are dying from COVID-19 at higher rates than other populations.
Northwestern Medicine cardiovascular experts discuss how racial disparities, including lower socioeconomic status and pre-existing cardiovascular conditions, can lead African-Americans to be at higher risk for contracting and dying from COVID-19.
Another example of health disparity
“This has really erupted into a very large commentary — almost a volatile discussion — about yet another evident example of health care disparities that don’t just happen by randomness,” said Dr. Clyde Yancy, chief of cardiology in the department of medicine and vice dean for diversity and inclusion at Northwestern University Feinberg School of Medicine. “We know the population we’re describing has a has high penetration of high blood pressure, obesity, diabetes, pre-existing cardiovascular disease, even heart failure.”
Yancy provided his viewpoint on COVID-19 and African Americans in a recent article for the Journal of the American Medical Association.
This population’s increased risk of coronavirus disease underscores the importance of social distancing, said Dr. Robert Bonow, professor of cardiology at Feinberg. But social distancing might not be feasible in many cases.
“It may not be possible for many who are on the edge of poverty to stay at home and not work when they’re already working two or three jobs just to maintain the family structure and put food on the table,” said Bonow, also the vice chair development and innovation in the department of medicine at Feinberg. “There are important social determinants that may explain why we’re seeing the inability to keep up with the public health recommendations, as urgent as they are.”
The privilege of distancing
Clyde Yancy
“In a number of major metro areas, with Chicago being number one, a disproportionate percent of people who are succumbing to or dying of the COVID-19 infection are in fact black or African-American, and the disproportionality is in the context of their representation in the community. Thirty percent of the community in Chicago is African-American and 70% of the deaths due to COVID-19 are black.

“You have to first pause and say maybe race is just describing that group that has all these co-factors that put people at risk. But beyond those co-factors, what is the additional risk that is attributable to the certain social determinants of health that certain black and African-American people face in their home communities? Is that not putting them at an even higher risk?
“The ability to do social distancing may in fact be a privilege. In certain communities where the population is dense — instead of a home built for two or four, there are six, eight, or 10 people living there — just the feasibility of social distancing was beyond anything that was possible. So now you have a circumstance in which the one community that already is beset with social determinants of health and have other diseases that put them at risk are unable, because of their living circumstances, to do the one strategy — the one strategy — that we know slows this down and might eventually put a halt to it: social distancing. It’s no surprise, then, that blacks or African Americans are coming in more frequently with COVID-19 symptoms or are developing complications more frequently and are having more adverse outcomes.”
Hydroxychloroquine and azithromycin
Robert Bonow
“We’re really concerned about the messages saying, ‘Just take it, it’s not going to hurt.’ There are, indeed, some cardiovascular complications, which are not that common if you give it to healthy people. But if you’re giving a medicine that can cause serious heart rhythm disturbances in healthy people to people who are already at risk of severe cardiac complications of COVID-19, which many times include the predisposition to these very same serious heart rhythm disturbances, you may be putting people who are really sick at even higher risk. That’s why there’s this push to get some data before we start saying everyone should take it.”
Clyde Yancy
“We know full well that hydroxychloroquine and azithromycin, an ordinary antibiotic, independently lead to cardiac complications that lead to heart rhythm irregularities, and the particular heart rhythm irregularities can be fatal. There is a lot to lose if you use hydroxychloroquine and azithromycin together empirically and it’s not part of some data capture, some clinical trials or some structured observational series. We know there are indeed cardiovascular risks. We can’t always anticipate in whom those complications will occur, but they will occur.”
Heart damage due to COVID-19
Clyde Yancy
“The truth of the matter is we really don’t know why or how it impacts the heart. You would like to think it’s as simple as the virus attacks the heart, but I’ve recently seen biopsy series that are not confirming myocarditis (inflammation of the heart muscle), per se, as the main driver. What’s been described is that precipitously, the heart muscle gets profoundly weak, irregular heart rhythms occur, the heart goes in a standstill, and that kind of cardiac arrest is very hard for resuscitation to be successful."
Robert Bonow
“It is common in 75- or 80-year-old persons who are undergoing a surgical procedure — gastrointestinal or orthopedic surgery — to find a couple days after surgery that there’s been evidence of injury to the heart. The stress of surgery sometimes can be a precipitant of cardiac injury. When you have severe pneumonia, such as influenza or COVID-19 infections, you have a similar situation of extra stress that can cause heart damage in susceptible individuals. With pneumonia, however, you’re also robbing the body of oxygen, which will also impair the heart of people who are at risk of heart failure or coronary disease.

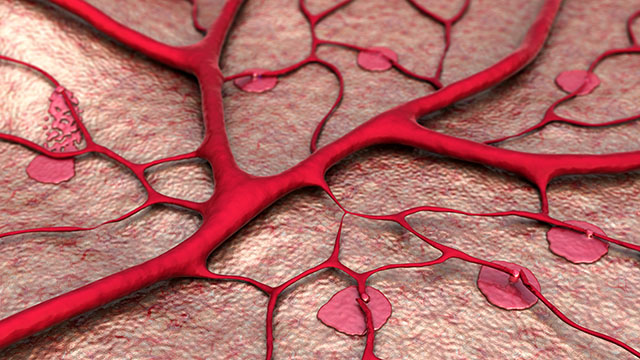
“Those are the baseline things, but then COVID-19 has some additional specific factors than can lead to heart complications. The surface of the virus has proteins that attach to receptors in the cells of the lungs, and those same receptors sit on blood vessels. So in addition to causing the effects of a severe pneumonias, COVID-19 may also have a direct effect on blood vessels that can lead to blood vessel damage including blood clots that can result in heart attacks. The cardiac complications of COVID-19 are complex and multi-factorial. And in any one person, there may be multiple aspects of this puzzle occurring at the same time — stress, lack of oxygen, blood vessel damage. And finally the body’s immune response, designed to fight infections can create an intense inflammatory responses in the setting of very severe infections which itself can be detrimental and result in damage to many organs including the lungs and the heart. This severe inflammatory reaction — often called “cytokine storm” — may occur in people of any age, including previously healthy young individuals.”