CHICAGO --- Multiple sclerosis (MS) may be triggered by the death of brain cells that make the insulation around nerve fibers, a surprising new view of the disease reported in a study from Northwestern Medicine and The University of Chicago. And a specially developed nanoparticle prevented MS even after the death of those brain cells, an experiment in the study showed.
The nanoparticles are being developed for clinical trials that could lead to new treatments -- without the side effects of current therapies -- in adults.
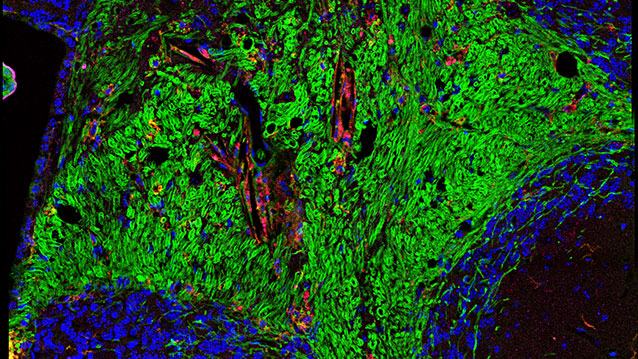
MS can be initiated when damage to the brain destroys the cells that make myelin, the scientists showed. Myelin is the insulating sheath around nerve fibers that enables nerve impulses to be transmitted. The death of these cells, oligodendrocytes, can activate the autoimmune response against myelin, which is the main feature of MS. Oligodendrocytes can possibly be destroyed by developmental abnormalities, viruses, bacterial toxins or environmental pollutants.
The scientists also developed the first mouse model of the progressive form of the autoimmune disease, which will enable the testing of new drugs against progressive MS. In the study, nanoparticles creating tolerance to the myelin antigen were administered and prevented progressive MS from developing.
The study was published in Nature Neuroscience December 14.
The lead investigators are Stephen Miller, Judy Gugenheim Research Professor of Microbiology-Immunology at Northwestern University Feinberg School of Medicine, and Brian Popko, the Jack Miller Professor of Neurological Disorders at the University of Chicago.
The nanoparticle technology was developed in Miller’s lab and has been licensed to Cour Pharmaceutical Development Company, which is developing the technology for human trials in autoimmune disease.
“We’re encouraged that immune tolerance induced with nanoparticles could stop disease progression in a model of chronic MS as efficiently as it can in progressive-remitting models of MS,” Miller said.
The timing of therapy is important, Popko pointed out.
“Protecting oligodendrocytes in susceptible individuals might help delay or prevent MS from initiating,” Popko said. “It’s likely that therapeutic strategies that intervene early in the disease process will have greater impact.”
In the experiment, scientists developed a genetically engineered mouse model in which the oligodendrocytes died, affecting the animals’ ability to walk. The central nervous system regenerated the myelin-producing cells, enabling the mice to walk again. But about six months later, the MS-like disease came barreling back. This demonstrated the scientists’ theory that the death of oligodendrocytes can initiate MS. In humans, the scientists posit, the disease develops years after the initial injury to the brain.
A molecular doppelganger
The current prevailing theory is that an event outside of the nervous system triggers MS in susceptible individuals who may have a genetic predisposition to the disease. In these individuals, the immune cells that normally fight infections confuse a component of the myelin sheath as foreign. These confused immune cells enter the brain and begin their mistaken attack on myelin, thus initiating MS.
New inside-out discovery
But the new study demonstrates the possibility that MS can begin from the inside out, in which damage to oligodendrocytes in the central nervous system can trigger an immune response directly. Oligodendrocytes are responsible for the maintenance of myelin. If they die, the myelin sheath falls apart. The inside-out hypothesis suggests that when myelin falls apart, the products of its degradation are presented to the immune system as foreign bodies or antigens. The immune system then erroneously views them as invaders and begins a full-scale attack on myelin, initiating MS.
An estimated 400,000 people in the U.S. and 2.5 million worldwide have MS. Of those with long-standing disease, 50 to 60 percent have progressive MS.
The other authors on the paper are Maria Traka of U of C, and Joseph Podojil and Derrick McCarthy of Northwestern.
Miller, a founder and chief of the scientific advisory board of Cour Pharmaceutical, does not receive financial compensation from the company.
The research was supported by grants from the Myelin Repair Foundation and the National Multiple Sclerosis Society.